-
Melanoma in darker skin tones: Race and sex play a role, Mayo study finds
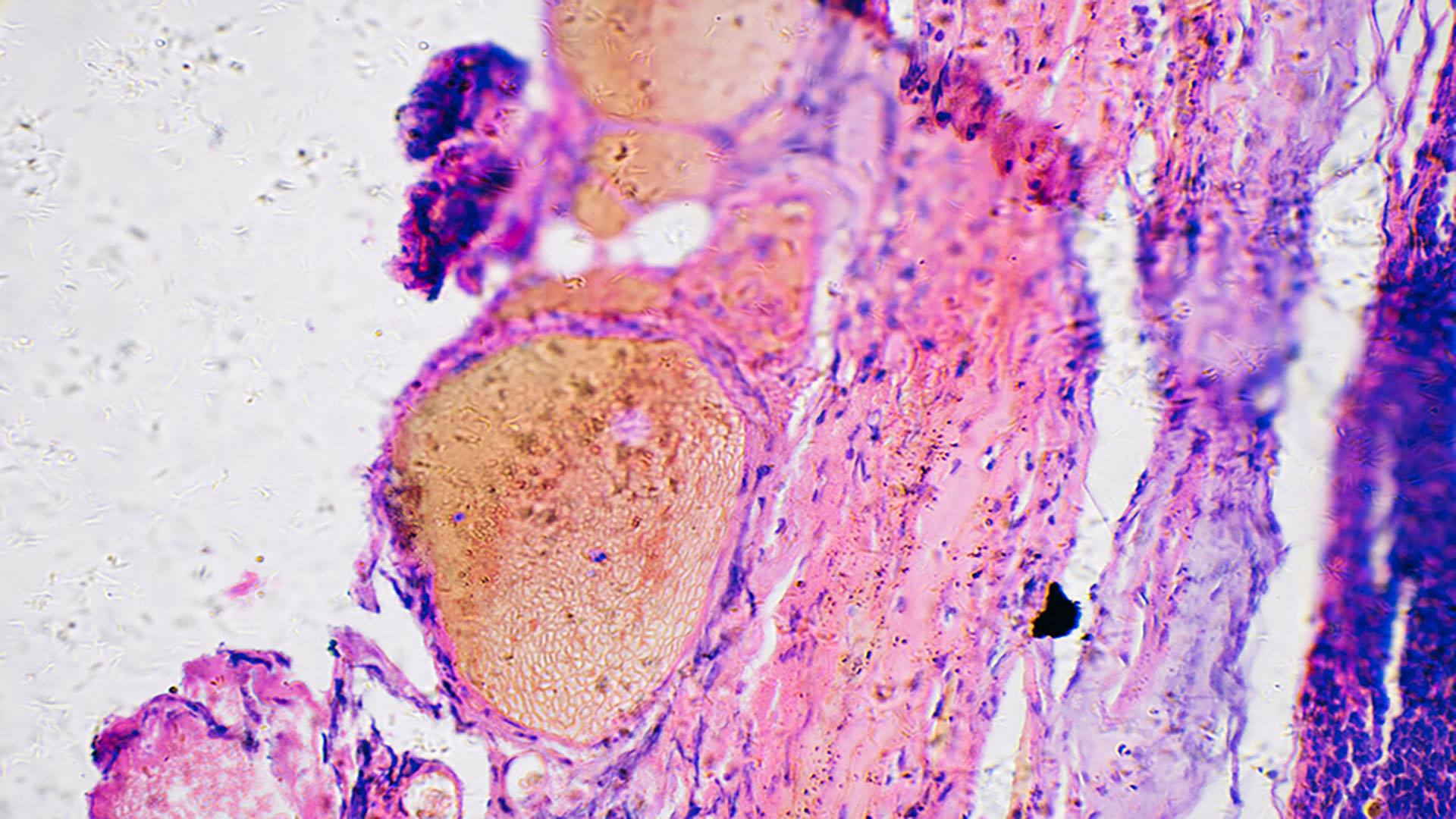
ROCHESTER, Minn. — Melanoma, an aggressive form of skin cancer that accounts for 75% of all skin-cancer-related deaths, is often detected later in people with darker skin complexions — and the consequences can be devastating, a Mayo Clinic study reveals.
While melanoma may be found less frequently in people with darker complexions than fair ones, this potentially serious form of cancer can strike anyone. The study, which consisted of 492,597 patients with melanoma, suggests that added vigilance in early screening is particularly needed for Black men, whose cancers are often found at later stages, leading to worse outcomes compared to white patients.

“We compared non-Hispanic Black patients to white patients and saw striking differences in how patients presented with the disease,” says surgical oncologist Tina Hieken, M.D., senior author of the study and a researcher at Mayo Clinic Comprehensive Cancer Center. “We saw more extremity melanoma, and more later-stage disease.”
Extremity melanoma refers to skin cancer that can develop on the arms, legs, hands and feet. Various factors, including social risk factors and biological components, could be at play, but further research is needed to help determine why these differences exist.
Revealing differences in sex-based immune response
The research found that Black female patients with melanoma fared better than Black male patients.
Men tended to be older at diagnosis and more likely to have cancer that had spread to their lymph nodes compared to women. This translated to worse survival rates. The researchers learned that Black men with stage 3 melanoma have only a 42% chance of surviving for five years, compared to 71% for Black women.
Most research on melanoma hasn’t focused on how race and sex affect outcomes and hasn’t looked at the influence of race and ethnicity across all groups. Dr. Hieken says the study highlights the need to understand these differences better, noting that this is the first large study to confirm that sex‐based differences in melanoma outcomes exist within the non-Hispanic Black population.
“When we talk about later-stage melanoma patients who are female versus male in that non-Hispanic Black patient cohort who ended up doing worse, some biological things may be going on here that are interesting,” says Dr. Hieken.
One theory centers on variations in immune response.
“Several immune signals suggest that women may respond better to some immunotherapies than males,” says Dr. Hieken.
Identifying the need
Researchers note that more studies focused on melanoma in a broader range of people, including more Black participants in clinical trials, is key to bridging this knowledge gap and potentially identifying more effective treatments.
“We want to broaden and deepen our reach to better understand the disease that affects all patients,” says Dr. Hieken.
She underscores the role played by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery in this study.
“What we’ve done with the Kern Center, with this study and others, is to identify the need,” says Dr. Hieken. “We have a rich, integrated, multidisciplinary clinical research practice in melanoma, and we want to address clinical needs and knowledge gaps relevant to our practice.”
A wake-up call in the battle against melanoma
Dr. Hieken notes that this study is a wake-up call for everyone battling to diagnose and cure melanoma, regardless of the patient’s sex or skin tone.
She emphasizes that healthcare professionals should carefully examine areas like palms, soles and under fingernails, where melanoma might be more challenging to spot on darker skin.
“We can incorporate screening for skin lesions or lesions under the nails into the visit for patients as part of their regular checkups,” says Dr. Hieken. “What we want to do is elevate care for our patients.”
The Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery and Breast and Melanoma Surgical Oncology in the Department of Surgery supported this research. Review the study for a complete list of authors, disclosures and funding.
###
About Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery
The Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery collaborates with clinical areas across Mayo to create and evaluate data-driven solutions to transform the experience of health and healthcare for patients, staff, and communities. It drives continuous improvement of Mayo Clinic as a learning health system, enabling always safe, evidence-based, high-quality care.
About Mayo Clinic Comprehensive Cancer Center
Designated as a comprehensive cancer center by the National Cancer Institute, Mayo Clinic Comprehensive Cancer Center is defining new boundaries in possibility, focusing on patient-centered care, developing novel treatments, training future generations of cancer experts and bringing cancer research to communities. At Mayo Clinic Comprehensive Cancer Center, a culture of innovation and collaboration is driving research breakthroughs that are changing approaches to cancer prevention, screening and treatment, and improving the lives of cancer survivors.
Media Contact:
- Vincent Jacobbi, Mayo Clinic Communications, newsbureau@mayo.edu
Learn more:
Mayo Clinic Minute: Melanoma misconception — dark skin tones at risk too
Mayo Clinic Minute: Men need to take melanoma seriously



