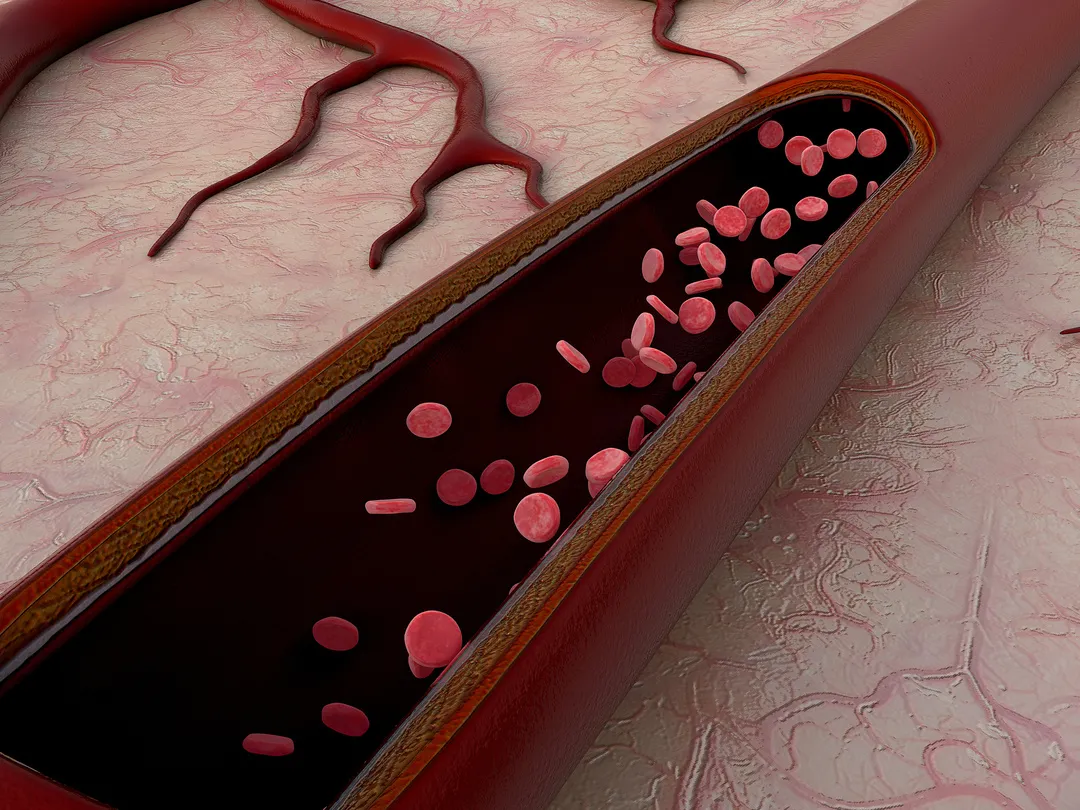
The blood vessels in the human body are like highways, and the platelets in the blood are like vehicles.
When platelets gather and clump together in the blood vessels for various reasons, they form blood clots, which block the highway. If the “vascular highway” becomes too narrow, causing “traffic jam” or “traffic flow slowdown”, then blood and nutrients will not reach all tissues and organs smoothly, which will cause local organ Ischemia, such as myocardial ischemia or cerebral ischemia. In case of severe and persistent “traffic jam”, i.e. continuous ischemia, it can lead to myocardial infarction and cerebral infarction. The anti-platelet aggregation drug aspirin can prevent platelets from “clumping together” inside the blood vessels, preventing the formation of blood clots. Therefore, in the prevention and treatment of cardiovascular and cerebrovascular diseases, aspirin often plays a big role, and its status is undeniable. However, in actual life, many patients with chronic diseases often forget the pain when they are well, or take a fluke mentality and pay less attention to long-term aspirin use, which eventually leads to adverse consequences are common. So, who needs to take aspirin? How to regulate the use?
A few days ago, Ge Caiying, chief physician and associate professor of general practice at Fangzhuang Community Health Center in Fengtai District, Beijing, was interviewed by a reporter.
At the beginning of the interview, Professor Ge shared a case she encountered in the clinic.
Case
The patient, Ms. Wang (pseudonym), is now 65 years old and has a history of hypertension, diabetes and hyperlipidemia, and has been seen here for many years. Two months ago, she entered my office and said to me with palpitations, “Do you know, Dr. Ge? We almost went bye-bye! I’m now turning my guts blue!” She said this, tears like a spring, snotty. I heard from a neighbor that taking aspirin can easily lead to stomach bleeding, so I inadvertently stopped taking it. Then one day, when I was carrying a bowl, I suddenly dropped it on the floor. I didn’t care at the time, I just thought how I was so careless, so unlucky. I didn’t expect that three days later, I suddenly clicked on the floor and instantly didn’t know anything. The ambulance arrived soon after, and I was conscious and didn’t feel uncomfortable, mainly because my face and scalp were broken. However, it did scare my family, so I went to the hospital for a CT and MRI, which showed no major problems. The doctor asked about my medical history and said that my blood pressure, blood sugar and lipids are currently under control, but it was the sudden discontinuation of aspirin that caused the two transient cerebral ischemic attacks.” Although the incident did not seem to leave any sequelae, it had a great psychological impact on Ms. Wang, leaving her in a state of panic and fear all day long. She thought about living alone, what if she collapsed one day and no one knew about her condition? Especially during the epidemic, she also did not dare to go out easily. The good thing is that after this incident, Ms. Wang began to follow the doctor’s advice and take regular medication, and now she has reached the control goal she wanted clinically. I also helped her with psychological counseling at a later stage, understanding her inner world by setting up a sand tray and psychologically guiding her, and she is now recovering well.
In fact, Ms. Wang’s case is quite typical in the clinic. Her experience has given us an inspiration: it is crucial to take aspirin regularly, and there are endless consequences if you stop taking it at will.
Who needs to take aspirin?
In cardiovascular disease management, there is the concept of primary prevention and secondary prevention.
Primary prevention refers to the use of measures to prevent the first thrombotic event in people who do not have atherosclerotic thromboembolic disease (e.g., coronary heart disease, ischemic stroke, peripheral arterial disease, etc.).
Secondary prevention refers to the prevention of disease progression, improvement of prognosis, reduction of death and disability, and prevention of recurrence through effective interventions in patients who have already developed coronary heart disease, ischemic stroke, and other atherosclerotic vascular diseases.
The 2019 Chinese Expert Consensus on the Use of Aspirin in Primary Prevention of Cardiovascular Diseases clearly states that aspirin can be used in eligible high-risk populations as primary prevention.
As for the specific medication regimen, it needs to be formulated by the physician taking into account a number of indicators such as blood pressure, blood glucose, blood lipids, and age.
In secondary prevention, the status of aspirin is unshakeable. In other words, for patients who have been diagnosed with atherosclerotic cardiovascular disease, they should follow medical advice to take aspirin for a long time.
Stopping the drug is dangerous and harmless?
It is indeed true.
Aspirin, as an anti-platelet aggregation drug, can prevent platelets from bunching up in the blood vessels, thus preventing thrombosis.
However, it needs to be taken by patients for a long time and regularly to achieve this effect. In other words, it can only work if the concentration of the drug in the blood is maintained for a long time.
Professor Ge also mentioned in the interview that “the inhibition of platelets by aspirin is a relatively long-lasting process, and this effect is sustained only if the patient keeps taking it every day.”
Therefore, if patients take aspirin at random and take it off and on, especially those who have had cardiovascular events such as myocardial infarction and angina pectoris, or are diagnosed with cardiovascular lesions, they are likely to be in danger.
As an example, the incidence and recurrence rate of cardiovascular events is clearly higher in patients who do not adhere to long-term aspirin use than in those who take the medication regularly.
How to think about gastrointestinal side effects
What should I do if I experience side effects?
The common side effects of aspirin are mainly bleeding tendency and gastrointestinal symptoms.
Professor Ge said, “In the clinic, although taking aspirin does have the side effect of gastrointestinal bleeding, the percentage is not high. Once gastrointestinal bleeding occurs, wait for the bleeding to end and take aspirin at the same time as a gastric mucosal protector proton pump antagonist.”
Usually, to avoid gastrointestinal discomfort, it is more recommended to take aspirin enteric tablets.
Enteric tablets have an enteric sugar coating on the outside, making them less likely to disintegrate in gastric juices, and the drug disintegrates and is absorbed into the intestine, which reduces the damage to the stomach.
Should I take it in the morning or in the evening? Is it taken on an empty stomach?
Professor Ge believes that “for this drug, it does not matter whether you take it in the morning or at night, there is no big difference, as long as you insist on taking it every day. Because its inhibition of platelets is a constant state, it is not limited by the time the drug is taken in the morning or evening. In addition, in order to reduce the stimulation of the stomach, it should be taken on an empty stomach.”
So, the most important thing is to stick to taking it every day, and it is rather secondary to which time of the day it is taken.
Professor Ge also reminded people that “when taking enteric tablets, it is recommended that you swallow them whole and not chew and crush them, otherwise it will lose its enteric effect.”
In addition, for the dosage, Professor Ge said, “the specific dosage, it is still recommended to go to the hospital to find a doctor to consult according to the individual situation. In primary prevention, the aspirin dose can fluctuate from 75 to 100 mg. At present, long-term aspirin enteric tablets of 100 mg a day are recommended.”